Abstract

Introduction Studies in 2-dose COVID-19 vaccinated hematology patients demonstrated reduced humoral immune responses compared to healthy individuals. It has become common practice to offer these patients a 3rd COVID-19 vaccination but data substantiating this are scarce. We quantitatively and qualitatively evaluated humoral as well as cellular responses to a 3-dose vaccination schedule, followed by a 4th vaccination, in a prospectively designed, large and diverse cohort of patients with hematologic malignancies.
Methods We prospectively quantified SARS-CoV-2-specific spike glycoprotein 1 immunoglobulin G (S1 IgG) concentration against the first serum standard for COVID-19 (20/136; provided by the National Institute for Biological Standards Control), antibody neutralization capacity of wild-type virus and variants of concern, and SARS-CoV-2-specific CD4+ and CD8+ T cell responses by activation marker expression, cytokine production and peptide-HLA tetramer staining in patients with hematologic malignancies prior to, and 4 weeks after each COVID-19 vaccination. Antibody concentrations were compared to those obtained by age-matched healthy individuals, extracted from a population-based study conducted by the Dutch National Institute for Public Health and the Environment. Previously infected participants, identified as having nucleocapsid (N) IgG >14.3 BAU/ml, were excluded from further analysis.
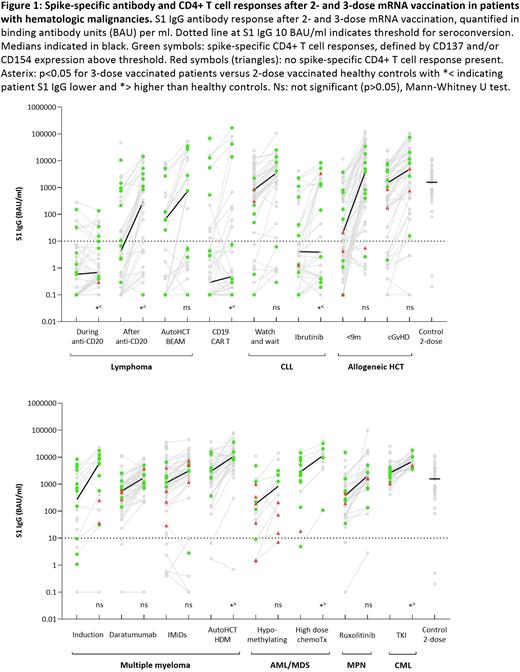
Results In total, 692 patients with a hematologic malignancy were included in the study. In 673 evaluable patients S1 IgG concentrations were significantly lower after the primary 2-dose mRNA-1273 schedule, compared to concentrations in age-matched healthy individuals (Haggenburg et al., Blood Adv 2022). A 3rd mRNA-1273 vaccination led to S1 IgG concentrations comparable to those obtained by age-matched healthy individuals after the primary 2-dose mRNA-1273 schedule (Figure 1). Moreover, a 3rd vaccination significantly improved antibody neutralization capacity against SARS-CoV-2 wild type and variants of concern (not shown). The rise in S1 IgG concentration after the 3rd vaccination was most pronounced in patients with a recovering immune system, but potent responses were also observed in patients with persistent immunodeficiencies. S1 IgG antibody concentrations remained low in patients receiving, or shortly after, anti-CD20 therapy, CD19-directed chimeric antigen receptor T cell therapy, and in chronic lymphocytic leukemia patients receiving ibrutinib (Figure 1; Haggenburg et al., medRxiv 2022). In most B cell depleted patients, spike-specific CD4+ and, most prominently, CD8+ T cell responses were generated. A dichotomy between humoral and cellular immune responses was also observed in other patient groups: patients with myeloproliferative disease receiving ruxolitinib, multiple myeloma patients receiving immunomodulatory drugs or daratumumab, and patients with chronic graft versus host disease obtained adequate S1 IgG concentrations, but less pronounced SARS-CoV-2-specific, cytokine-producing CD4+ and/or CD8+ T cell responses after each vaccination. This is in contrast to multiple myeloma patients receiving 1st line remission-induction therapy followed by high-dose melphalan and autologous HCT, who generated antibody and CD4+ T cell responses comparable to healthy individuals. In patients with myeloid disease receiving hypomethylating agents S1 IgG antibody and T cell responses were both impaired. A 4th vaccination further improved S1 IgG concentrations in the majority of patients; its effect on cellular immunity is currently being evaluated.
Conclusion After a 3-dose mRNA vaccination schedule, the majority of patients with hematologic malignancies obtained adequate antibody concentrations and robust CD4+ T cell responses. However, T and B cell responses were often discordant: the presence of adequate SARS-CoV-2 specific antibody concentrations was not necessarily accompanied by robust T cell immunity and vice versa. The impact of discordant T and B cell responses on vaccine effectiveness requires further investigation.
Disclosures
Zweegman:Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees. Kater:Abbvie: Membership on an entity's Board of Directors or advisory committees, Other: speakers fee, Research Funding; Astra Zeneca: Membership on an entity's Board of Directors or advisory committees, Other: speakers fee, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees, Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees, Other: speakers fee, Patents & Royalties: pending, Research Funding; Roche/genentech: Membership on an entity's Board of Directors or advisory committees; LAVA: Membership on an entity's Board of Directors or advisory committees, Patents & Royalties: pending. van Meerten:Kite, a Gilead Company: Consultancy, Honoraria; Janssen: Consultancy; Celgene/BMS: Research Funding; Genentech: Research Funding. Mutsaers:Astra Zeneca: Research Funding; GSK: Consultancy; BMS: Consultancy.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal